Transcranial magnetic stimulation (TMS) is a breakthrough treatment for patients with depression who do not find relief from their symptoms with antidepressants. There are currently seven FDA-approved TMS machines used in clinics across the US. Madison Avenue TMS & Psychiatry is proud to announce that, in addition to the NeuroStar®…
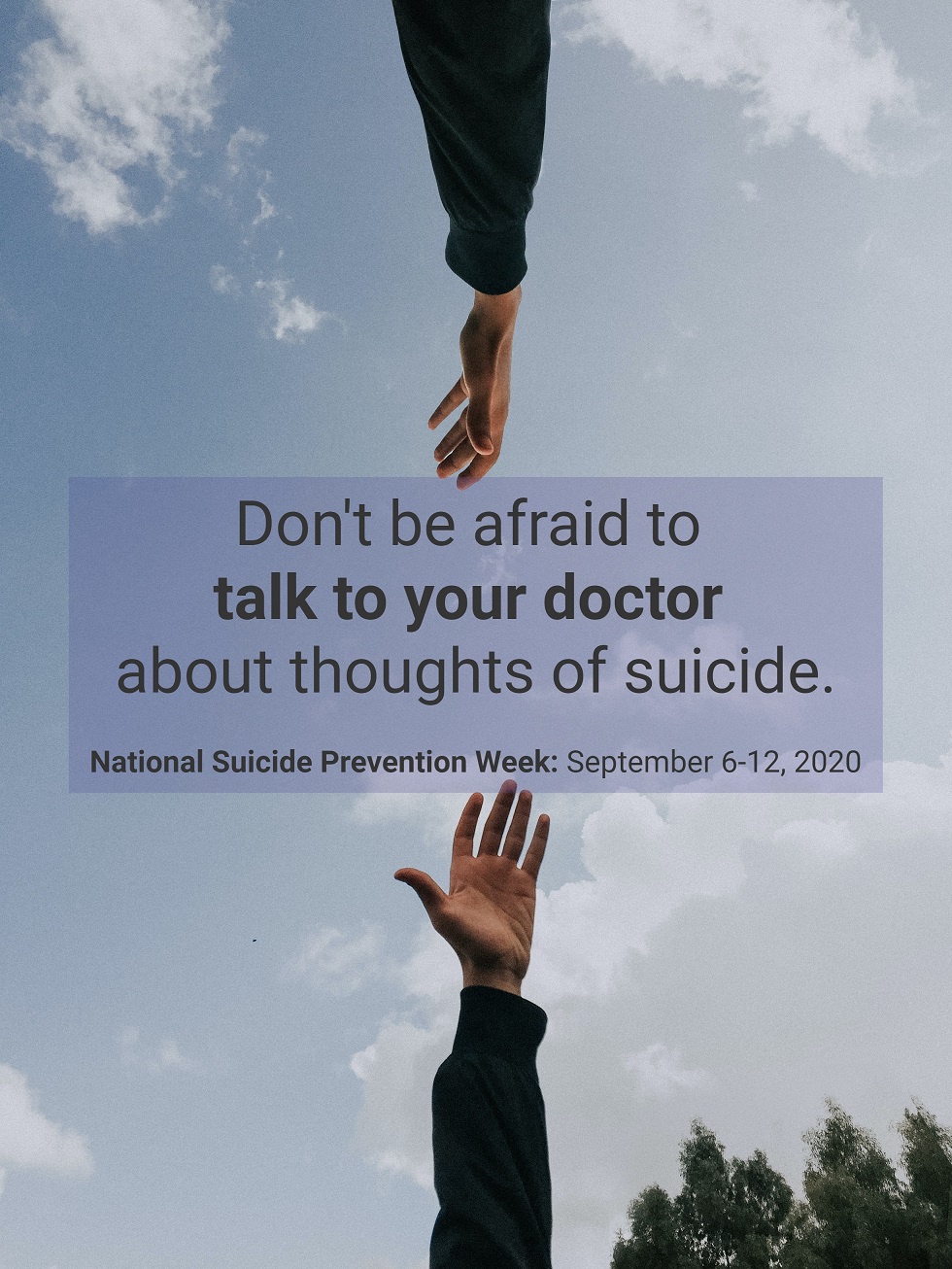
Many people who struggle with thoughts of suicide are afraid to tell a healthcare provider because they’re worried they’ll immediately be involuntarily committed to a psychiatric facility. This is not the case. Suicidal ideation is a symptom of a mental health disorder, and just like any other symptom, it’s important…
As of Monday, July 13, we’ve reopened our doors and are thrilled to offer TMS again. We’re now accepting new patients, as well as new appointments for existing patients. Please call us at (212) 731-2033 or contact us online to make an appointment. Our COVID-19 Safety Precautions Our #1 priority…
Suicidal thoughts, also referred to as suicidal ideation, and suicide affect men and women of all ages and ethnicities around the world. The most recent reports given by The Centers for Disease Control and Prevention report that suicide is the tenth leading cause of death in the general population and…
May is Mental Health Awareness Month
May 16, 2019
Learn How You Can Make a Difference Mental Health Awareness Month is a time of the year dedicated to raising awareness about mental health conditions in order to reduce the stigma surrounding them, promote practices that support emotional well-being, and to encourage more people suffering from mental health conditions to…
We are happy to announce that Dr. Woo will be attending the Clinical TMS Society’s annual meeting of 2019 in Vancouver from Thursday, February 21 until Saturday, February 23. This gathering of TMS researchers, industry experts, and the most experienced providers of transcranial magnetic stimulation is world-renowned for its workshops, demonstrations,…